Pelvic Floor Physical Therapy Specialty Offered at Memorial
When most people hear the words “physical therapy,” they likely associate it with treatment needed following an injury, surgery, stroke, paralysis or another type of trauma that limits one’s ability to function normally.
However, there are a variety of specializations physical therapists can pursue to assist patients experiencing very specific issues.
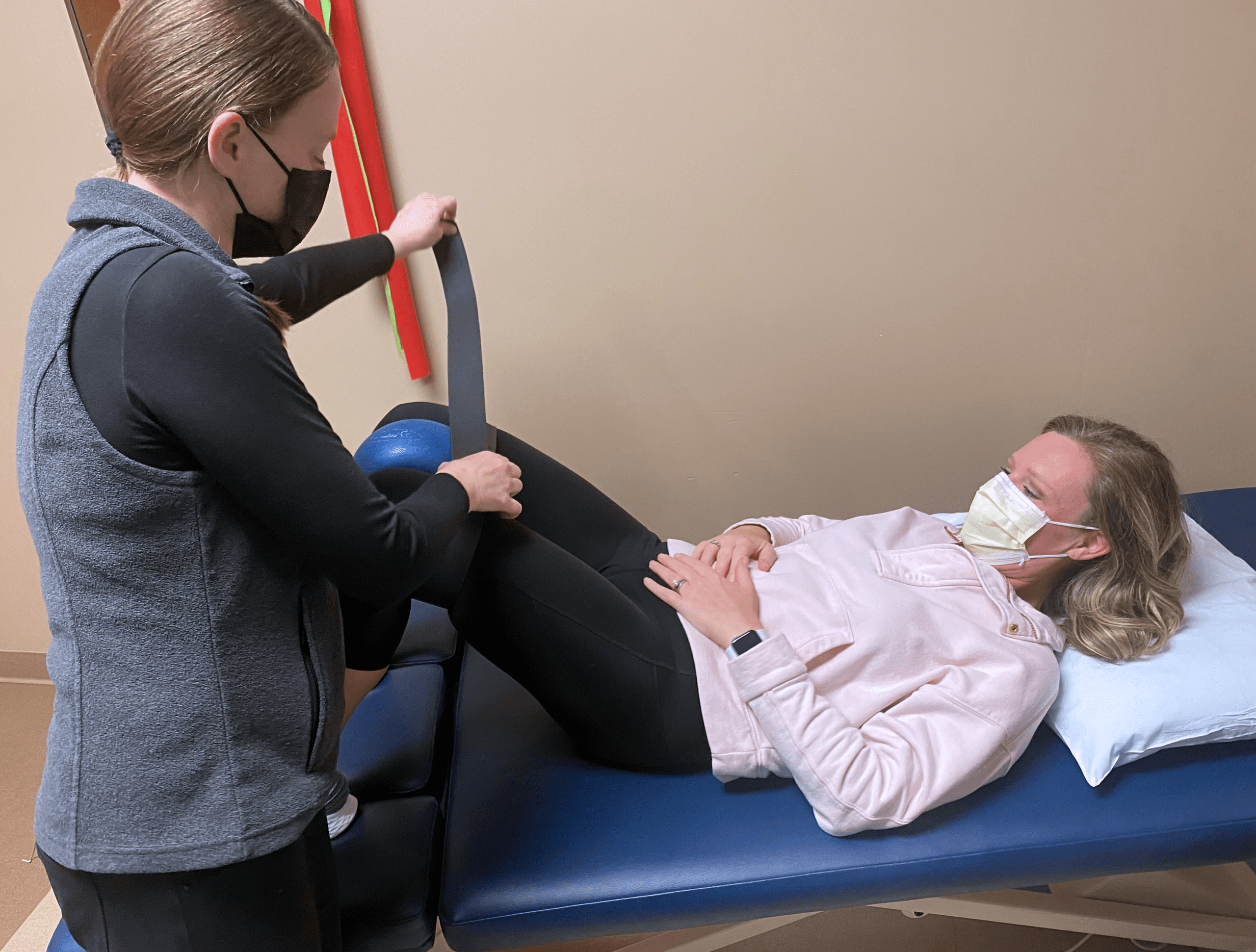
Kay Descher, physical therapist at Memorial, has specialized in Pelvic Floor Physical Therapy (PFPT) for 20 years.
“I started working as a PFPT 20 years ago, and it has been awesome to watch the increased referrals over these past two decades,” she said. “Social media has helped take away some of the taboo of PFPT, and it helps individuals feel more comfortable seeking the help they need. Pelvic floor health is an important part of mental well-being as well as physical comfort.”
Descher said she works with patients to correct pelvic malalignments –placing the pelvic floor muscles into better position, myofascial release that helps relieve connective tissue restrictions and pain, bowel conditions in adults and children, pelvic floor muscle tone issues, urinary incontinence and pelvic organ prolapse symptom management, among others.
Jessica Lotz, PFPT patient, experienced some unexplained bladder issues and decided she wanted to try pelvic floor therapy.
“My physician said, ‘I’m not sure it will help like you’re hoping it will, but let’s give it a try’,” she said. “Having followed a few medical accounts on Instagram and identifying with some of the posts about dysfunctional pelvic floors, I wanted to give pelvic floor therapy a try.”
Lotz said her symptoms included urinary frequency, urgency, pain with voiding and a burning sensation in her bladder. She said doctors told her that the symptoms all pointed to recurrent urinary tract infections (UTIs), but the tests kept coming back negative for infection.
“The days were difficult leading up to a diagnosis,” she said. “Within the first few minutes of my initial consult with Kay, I felt confident that this therapy would provide symptom relief. Kay asked good questions and was an excellent listener.”
Lotz said one way Descher helped her at the beginning was with a thorough explanation of the physiological structure of the pelvis, including how the pelvic floor works with our internal organs.
“The pelvic floor muscles sit within the base of the pelvis,” Descher said. “It is the floor of the core system that supports your skeleton. It supports the internal organs of the pelvis and abdomen and assists with bowel/bladder elimination and sexual function.”
Lotz said that after Descher reviewed her past medical history, including five abdominal surgeries, and performed a physical exam, she was diagnosed with Hypertonic Pelvic Floor Disorder or dysfunction.
“This dysfunction causes the pelvic floor muscles to be overly tight, and it inhibits the body’s ability to perform at its optimal level,” Descher said. “Most women and men will experience this dysfunction in their lifetime.”
Rather than her pelvic floor muscles being long, flexible and relaxed, Lotz said hers were short, tight and sat higher in her pelvis than they should.
“Imagine flexing your bicep all day, every day,” she said. “That was my pelvic floor. The constant contraction created a number of problems, including bladder discomfort. Most people carry their stress in their neck, shoulders or back. As it turns out, I carry my stress in my pelvic floor. Stress combined with my surgical history and endometriosis likely contributed to years of inadvertent muscle tension, shortening my pelvic floor.”
Descher said everyone holds stress within their bodies, and the pelvic floor muscle is a common place.
“I call this postural tension,” she said. “For example, we all have muscles that help us sit at a desk. Let’s say we are having more stress that day, and we start tightening other muscles that we don’t need to tighten while sitting. This could be elevated shoulders, holding your abdomen in, tightening your glutes or tightening your pelvic floor. When we are in pain, we tend to tighten our muscles as a guarding mechanism. When my patients become aware of this excess tension, I instruct them to let the tension go.”
Lotz said that working with Descher brought awareness to just how tense she was without even realizing it, and she experienced immediate relief the first time she was able to let go of the tension in her pelvic floor. Through a physical exam and a muscle movement sensor, they found that Lotz had lost the connection between the brain and pelvic floor muscle.
“Biofeedback showed that I had poor muscle control,” Lotz said. “I could contract on demand, but the muscle took longer to release and required a very intentional focus in order to relax. It took several months of in-office therapy and at-home exercises to gain muscle control and switch from a state of constant contraction to a more frequent state of relaxation.”
Physical therapy for Lotz included internal trigger point work, electrical muscle stimulation, deep breathing exercises and stretching.
“I remember being surprised at how minor some of the exercises seemed,” she said. “They were not physically challenging, per-se, but rather small, intentional movements aimed at increasing muscle control, which eventually lengthened and lowered my pelvic floor to its normal resting tone. I was surprised at how physical therapy turned out to be very mentally challenging for me.”
Descher said she tells her patients that the pelvic floor muscle is an emotional muscle, so it makes sense that physical therapy would be more mentally draining.
“This muscle has so many functions, and if one of those functions is disrupted, the result can be emotionally isolating,” she said. “It can also be draining because it takes a lot of focus to be able to give the pelvic floor the correct input to affectively contract and relax.”
Lotz said that learning to go from her body’s default state of tension to being aware and focusing on intentional muscle relaxation was difficult.
“Spending an hour per week in physical therapy was fairly easy compared to the intentionality I have to bring into my daily life in order to maintain muscle control and tone.”
After years of unexplained urinary symptoms and frustration, Lotz said she feels fortunate to have found Descher and the relief she provided through PFPT.
“Working with her helped me understand how the pelvic pressure, bladder pain and hip immobility and discomfort I felt for years was due to hypertonic pelvic floor disorder,” Lotz said. “My hope is that others hear about this relatively underutilized therapy and consider if it’s an option for them as well.”
Descher said she works with pelvic floor patients about 90 percent of the time and has seen an increase in the therapy’s popularity over the course of her career. She said her next educational endeavor is working toward her certification in visceral manipulation, a gentle organ-specific myofascial release technique for improving organ functionality, mobility and motility.
All PFPT sessions are completed in a private treatment room with one therapist. For more information, you can visit Memorial’s Pelvic Floor Dysfunction web page at https://ortho-neurocenter.org/pelvic-floor-dysfunction/